Houston’s Urban Efforts to Combat Childhood Obesity

Houston tackles childhood obesity through multi-pronged urban initiatives addressing its roughly 31% adult obesity rate and high youth rates. You'll find school programs like CAN DO Houston offering fitness activities and nutrition education, alongside community partnerships targeting underserved neighborhoods with culturally responsive approaches.
Recent federal nutrition standards for school meals are reducing added sugars and limiting high-sugar foods. These coordinated efforts aim to close the health gap affecting Hispanic and African American children disproportionately. Discover how these strategies are transforming young lives across the city.
The Alarming Rise of Childhood Obesity in Houston: Statistical Overview
While national childhood obesity rates remain concerning, Houston faces an even more troubling reality. With Texas ranking among the highest states for youth obesity nationally (around fifth for ages 10–17), Houston-area children face elevated risks that mirror the county's adult obesity rate—significantly above the national average.
Lower-income neighborhoods show substantially higher obesity rates than affluent areas. Contributing factors include sedentary lifestyles, with decreased physical activity and increased screen time, alongside sleep deprivation which disrupts metabolic processes. The prevalence of about 1 in 4 school-aged children in Texas having obesity highlights the severity of this public health crisis.
Despite limited city-specific data, the upward trend in Harris County suggests Houston's children face persistent challenges that demand targeted urban interventions.
You'll find stark disparities across communities, with Hispanic and African American children experiencing nearly twice the obesity rates of their white peers in Texas and the Houston area.
Health Consequences of Obesity for Houston's Youth
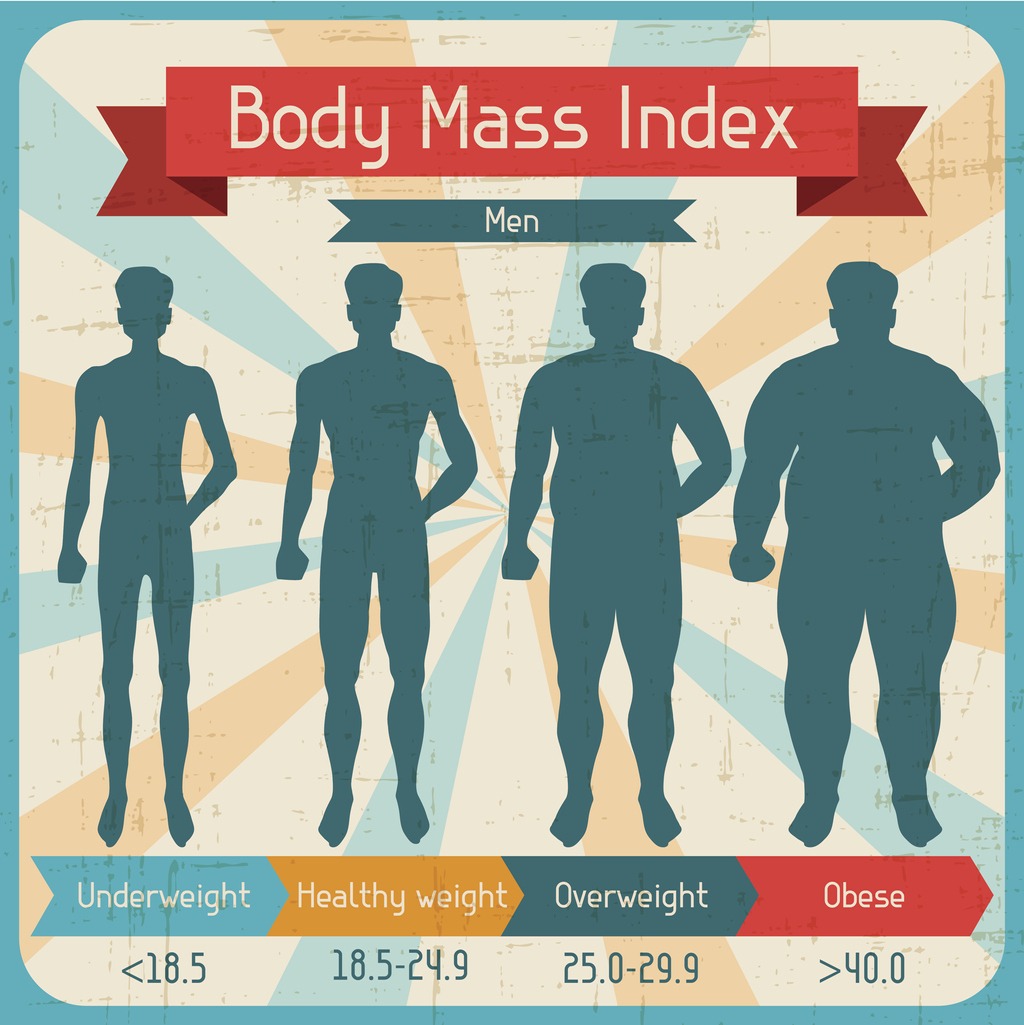
As Houston's childhood obesity rates climb, the health implications for affected youth extend far beyond cosmetic concerns. Overweight children face immediate physical challenges and long-term health risks that can reduce their life expectancy by 5–20 years.
You'll notice these serious consequences in affected children:
- Chronic disease development—including type 2 diabetes, hypertension, and fatty liver disease—appearing at increasingly younger ages
- Decreased physical mobility due to joint pain, reduced exercise tolerance, and musculoskeletal issues that create a cycle of further inactivity
- Increased mental health risks manifesting as depression, anxiety, and lower self-esteem, often exacerbated by social stigma and exclusion
The economic impact is equally concerning, with medical costs for children with obesity exceeding those of normal-weight peers by up to $19,000 over their lifetime, rather than annually. This burden is particularly heavy on Houston's Hispanic and African American children, who experience nearly twice the obesity rate compared to their non-Hispanic white peers.
School-Based Programs Transforming Student Health
View this post on Instagram
Houston schools have emerged as powerful frontlines in the battle against childhood obesity, implementing innovative programs that address both nutrition and physical activity where children spend most of their day. Programs like CAN DO Houston coordinate with school districts to offer after-school fitness sessions, nutrition education, and school gardens that engage hundreds of students and families in priority neighborhoods. Following the CDC’s Coordinated School Health model, these initiatives include peer-led health education and school cafeteria interventions tailored to Hispanic and Black student populations. Evidence-based Texas programs such as the CATCH model and Texas GROW! EAT! GO! integrate walking programs with family gardening, while digital platforms enhance student engagement and inform local efforts in the Houston region. The organization works with more than 60 organizations in Houston to facilitate collaboration and implement sustainable initiatives addressing childhood obesity. Parent cooking classes and staff wellness clubs create supportive environments, with preliminary findings showing increased physical activity and better nutrition awareness among participants. Beyond classroom walls, strategic community initiatives have emerged as essential tools in Houston's fight against childhood obesity, particularly in underserved neighborhoods where health disparities are most pronounced. Harris County Public Health and partner organizations focus on Hispanic and non-Hispanic Black children who face obesity rates substantially higher—often nearly twice those of their white peers—using culturally responsive practices to overcome barriers. These disadvantaged communities have less access to healthy resources that could help prevent childhood obesity. Three standout approaches making an impact: While community programs provide essential support, strategic policy changes have proven equally crucial in reshaping children's nutritional environments across Houston. You'll see the impact of Texas and federal nutrition policies, though childhood obesity rates indicate more work is needed. The USDA’s updated school nutrition standards, finalized in April 2024 and taking effect beginning with the 2025–26 school year, will significantly improve school meals by reducing added sugars, limiting high-sugar cereals, and controlling sodium levels. These changes matter because schools provide up to half of many children's daily nutrition. Starting in Fall 2025, flavored milk limits will be implemented with a maximum of 10 grams of added sugar per 8 fluid ounces, and similar product-based limits will apply to yogurt and breakfast cereals. Intersectoral partnerships between clinical providers like Texas Children’s Hospital and community organizations strengthen these efforts. Increased funding for programs like CATCH creates coordinated environments across education, food service, and physical activity domains, ensuring policy improvements translate to healthier children. Deeply entrenched within Houston's childhood obesity crisis lies a troubling pattern of socioeconomic inequality that demands urgent attention. Latino children in Houston face a 34% obesity rate compared to 26% nationwide, with up to 50% at risk for Type 2 diabetes over their lifetime. These disparities stem from systemic inequities that affect low-income families' access to health resources. Nearly one in three of Houston's children live below the poverty line, affecting their access to nutritious foods and safe spaces for physical activity. Nutritious foods are less common in low-income neighborhoods, making healthier dietary choices especially challenging for vulnerable families, and recent research shows that almost 39% of Harris County households experience food insecurity, with even higher rates among Black and Hispanic households. Community-based health interventions tailored to cultural needs have shown promising results, especially when engaging families directly. Nutrition education programs in lower-income neighborhoods help bridge knowledge gaps while addressing the realities of food insecurity.Community Initiatives Targeting Underserved Neighborhoods
Policy Changes Making an Impact on Children's Nutrition
Addressing Socioeconomic Disparities in Childhood Obesity